A discovery redefines biomedicine

James Thomson
For the first time, we had unlimited access to all of the basic cellular building blocks of the human body. And if you make an embryonic stem cell line, that’s infinite. You can make as many cells as you want.

Jeffrey Jones
At the time, there were people all over the world trying to do what Jamie did with human cells, and nobody could do it. Not only did you have to isolate these cells, but you have to be able to propagate them and keep them alive.

Jessica Antosiewicz-Bourget
What a discovery. There was a big sense of pride in the lab and a real sense of camaraderie, even though a lot of us only started shortly before the discovery was published. I remember reading the paper and just being blown away by the potential and how lucky I was to work in this field that was going to have such an impact in the future.

Carl Gulbrandsen
It was apparent that this was an incredibly important discovery. Having access to human embryonic stem cells permitted scientists, for the first time, to directly study cellular changes that occur in early human development.

Terry Devitt
We understood at an early stage this was going to be big news, and we needed to be ready as an institution. Months before the paper was published, I began working very closely with Jamie, getting my education in stem cell biology. What were these cells, why were they important, what were the ethical implications?

James Thomson
Before the human ES cell paper came out, I told [Terry Devitt] about it and he went through a little training course on how to deal with the media. Then I sat in his office for about two weeks where I did nothing but answer the phone, and I went through hundreds and hundreds of interviews in the basement of Bascom. When they were collecting the media articles, they started measuring it by foot of paper instead of number of articles.

Terry Devitt
It’s hard to predict the fate of news. I don’t think we realized it would be a story that would be front page news for years, decades. The stem cell story manifested itself in so many ways - scientific breakthrough, political drama, the business of stem cells, ethical conundrum. It is all of those things.

Virginia Hinshaw
Jamie's discovery was truly momentous. There are times in life where you realize you have to give your all, and 1998 was just such a time. I made a statement to the UW Regents saying 'this work holds great promise for the future, in understanding developmental biology, responses of cells to different drug therapies, and potentially generating tissues to replace diseased or damaged tissues in humans.' That was true then, and it's true today.

Gordon Keller
We and a handful of other people were differentiating mouse ES cells, and there was modest enthusiasm, but not much. Once Jamie's discovery was announced, once he identified human cells, it literally changed overnight what we thought we could to do with these cells.

Janet Rossant
The transition from mouse embryonic stem cells to human embryonic stem cells was a big breakthrough and a fundamental shift. Now we have stem cells with this capacity to make every cell type in the body. Can we harness that capacity?

Rupa Sridharan
We know from Jamie's work that pluripotency is a special state. That’s because most cells of our body can perform only one function, which is the whole point of development. We want our lungs to breathe, we want our liver to detoxify—we want them to have these specialized functions. But ES cells represent a blank slate. They are able to differentiate to be whatever you want them to be.
Getting it right: An early focus on ethics
All of the stem cell lines Thomson derived came from embryos donated by patients using in vitro fertilization clinics. These were excess embryos that would otherwise be discarded, but — with the consent of the donors—were instead given to research purposes.

Norm Fost
The initial reaction to almost any new technology leads to an initial fear and loathing opposition. It's not like it's the first time in the history of the world you could change human development, but this seemed like it would be such a powerful technology that it scared people. The world is coming to an end as we know it, and what does this mean?

Alta Charo
There was some degree of reaction to, I think, embryo research overall and not just to Jamie's research in particular. I got lots of unsolicited emails and letters. I had a lot of people praying for my soul. I had a few people condemning my soul. Then the occasional letter from patients who were grateful that the work was being done.

James Thomson
I think there are tremendous parallels between the early days of recombinant DNA research and the early days of stem cell research. Both created a big social uproar over whether we should be doing this, followed by a compromise, then moving forward with the research.

Alta Charo
Jamie called me out of the blue when he was still working with non-human primates. I had been on the NIH human embryo panel in '93, '94, and he must have figured that out somehow. He invited me to his lab, gave me a tutorial on embryonic stem cells, and explained why he might want to move from non-human primate to human primate. He wanted to know what ethical questions to be thinking about in advance.

Norm Fost
It's rare in science that the scientists look for somebody to slow them down. I remember Jamie said explicitly, ‘I'm not looking for how to spin this or how to head off criticism. I want to do it right.’ This was four years before he published his first human papers.
Federal restrictions and the launch of WiCell

Carl Gulbrandsen
It was dicey for Jamie to be doing this research at the university, because there's virtually no laboratory at UW–Madison that doesn't have some federal money in it. We came around to the notion that WARF should put together a private laboratory and fund it. The first laboratory with WiCell was 1200 square feet and on the second floor of an old AT&T switching station.

Robert Drape
Right away, WiCell's mission was to provide a safe haven for researchers to engage in stem cell research off of campus, but it also provided a venue for researchers — including some who weren't necessarily engaged in regenerative medicine — to receive training on stem cell culture techniques. Many people say culturing stem cells is an art. WiCell provided a real collaborative atmosphere for scientists to work together and learn the art from others.

Carl Gulbrandsen
The work WiCell did training researchers and making sure that they had success with the cells, that more than anything, I think, helped push the science forward. They're considered essentially the gold standard in the world for stem cell banks, and for the technology that they have.

Palmer Yu
It can be difficult to keep embryonic stem cells happy. They have the potential to differentiate to all the other cell types, and if you aren’t careful, they’ll start to spontaneously do so without direction from the scientist. It's actually a constant challenge for us to keep all cells in our culture, in a petri dish, in that undifferentiated state.
A political compromise and a way forward

Alta Charo
Some of the technical issues [with stem cells] were novel, but the one thing that there was precedent for, by contrast, was the political controversy. Everybody anticipated it was going to be a signature issue for the Bush administration, because it had been a major campaign issue.

Norm Fost
What was Bush going to say in that speech? It was on the front pages of the paper every day for months and months. I certainly didn't anticipate the particular way that the Bush administration threaded the needle.

Carl Gulbrandsen
We met with Wisconsin Gov. Tommy Thompson who was at a point in his career where he'd gotten interested in technology. He was fascinated with Jamie’s work and could understand the importance of it. Tommy went to NIH [when appointed Health and Human Services Secretary] and convinced Bush that they had to provide some federal funding for human embryonic stem cells.

Anita BHATTACHARYYA
His influence was really important. Thompson was amazingly supportive of the science, and it was great that he continued that support when he went to Washington.

Gov. Tommy Thompson
The president, after a cabinet meeting, said ‘Tommy, I've got to learn more about stem cells. You're for it, and Karl Rove is adamantly opposed to it. So I want you to come in for lunch and have a little debate, a discussion with you, Karl and myself.’ There was a little anteroom that was turned into a place to have lunch. I still remember the president had a peanut butter and jelly sandwich, and I had a hamburger.
I told the president that he had just doubled the amount of money going into NIH, and he had put a lot of money in for cancer. But all that good would go by the wayside. He would always be remembered as the individual that stopped science, if he prevented stem cell research from going forward. Everybody knows someone—a child, loved one, friend—who's suffering from a debilitating disease, and they expected embryonic stem cells to be the panacea. The savior.

Jessica Antosiewicz-Bourget
I remember I was working by myself in the lab early in the morning with the radio on, when the program started talking about the Bush decision on stem cells being announced that night. It was surreal, sitting at the hood, doing my work, and thinking about all the fuss caused by this little plate of cells.
August 9, 2001

Carl Gulbrandsen
They came up with a compromise that they would only fund existing cell lines. Which were our lines. There weren't many others.

Norm Fost
It was very interesting watching the scientific community struggle with whether they were going to celebrate that there was still a crack in the door or complain that the door had not been flung open the way they thought it should.

Gov. Tommy Thompson
Not everybody liked the compromise, but I did. That compromise was the breakthrough that got us to where we are today, which is a very fertile science that continues to show great promise.
Growth of the science at UW–Madison

Robert Drape
It's fun going to meetings and talking to people in the stem cell community that have never been to Madison. They refer to Madison as ground zero for stem cell research, the stem cell research hub. The exceptional quality of the academic research and industry in Madison continues to be recognized globally.

Igor Slukvin
Shortly after Jamie's discovery, we had groups established that study differentiation of pluripotent stem cells to things like neural, heart, pancreatic and blood cells. Embryonic stem cells came from UW and it brought the university to the forefront of stem cell research in the world.

David Gamm
The UW scientific community is one that's very open and collaborative and encouraging. We’re all part of a bigger machine and help each other out. There's a lot we can learn from one another and we're very open to sharing those ideas and successes and failures.
August 20, 2001
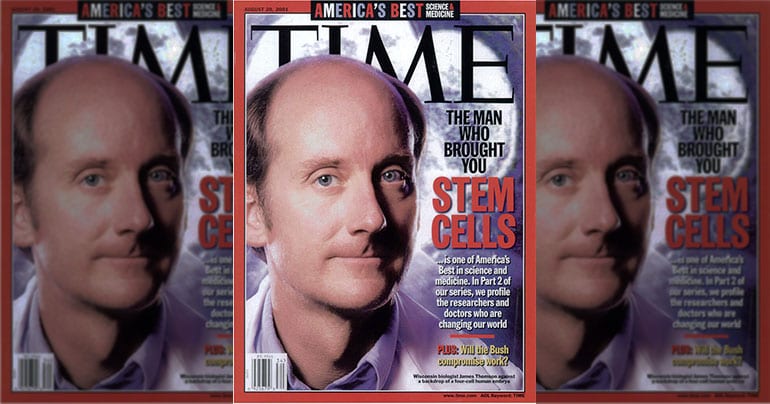
James Thomson, and the science of stem cells, is featured on the cover of Time magazine as part of their series on America’s Best in science and medicine.

Rupa Sridharan
I came to UW to start my own lab because it's such a good place to do stem cell research, and there's so much going on with both the basic and translational aspects. My lab is trying to figure out the special kinds of epigenetic controls that are found exclusively in pluripotent cells that makes them remain pluripotent.

Bill Murphy
We've worked on this brain organoid project, in which the idea was to create a predictive model for neurodevelopmental toxicity screening. If we could generate mimics of the human brain, we could expose those brain mimics to known compounds, measure their gene expression and feed it into a machine learning system. We could then use this to test the toxicity of unknown compounds.

Igor Slukvin
The major goal of our work is to advance the use of pluripotent stem cells for blood transfusion and treating blood cancer and genetic blood diseases. Instead of getting blood cells from donors, we hope to establish technologies for large scale production of blood cells so different blood components can be manufactured in factories and distributed to the hospitals.

Anita BHATTACHARYYA
My lab studies Down syndrome and Fragile X syndrome, a genetic form of autism. We know that the intellectual disability occurs because something went wrong in brain development. We’re using disease model stem cells to ask ‘what is it that goes wrong?’ I feel very strongly that to answer these questions we need human cells, and stem cells are the perfect paradigm.

David Gamm
I came to UW shortly after Jamie's groundbreaking discovery for ES cells, and there was really nobody working on stem cell applications in the eye at the time. We're now the first to describe a way to make a 3D retinal structure or organoids from human cells. Our work is trying to understand human retinal development both for modeling disease and for transplantation purposes.
Tim Kamp
Our research involves understanding the electrical properties of the heart and how they go wrong and cause arrhythmias. Because of my interactions with Jamie and early collaboration with him, we started using stem cells to derive cardiomyocytes. The nice thing is it's not too hard to tell if you have success with the cardiac differentiation, because when your cultures start beating, that's a pretty good sign.

Thomas Zwaka
I was working in Germany as a medical doctor, but was really interested in doing my own research project. I thought, maybe it's not a bad idea to ask Jamie if I could join his lab for a period of time, like a post doc. I worked on developing a gene editing technique, manipulating the genome in a targeted, very specific fashion. I focused on Oct-4, a transcription factor only present in pluripotent cells. So it's a good marker that allows you to tell, is this really a stem cell? Years later, Shinya Yamanaka and Jamie used this transcription factor, among others, to reprogram cells and make iPS cells.
The next big frontier: Adult stem cells
November 30, 2007

The journal Cell publishes Shinya Yamanaka’s work on successful reprogramming of human somatic cells into stem cells, known as induced pluripotent stem (iPS) cells. Thomson’s concurrent discovery of human iPS cells, with scientist Junying Yu, was published at the same time in Science.

Shinya Yamanaka
Jamie’s discovery that showed the potential for regenerative medicine had a tremendous impact on stem cell research. Because of Jamie's work, I started a project to make pluripotent stem cells directly from adult human cells. Jamie is the father of human ES cells. Without his contribution, we could never have generated human iPS cells.

James Thomson
IPS cells are something that anybody can make easily without all the ethical constraints of using human embryos. They’re basically the same exact cells, just a different source, and the number of people working in this field has exploded dramatically.

Anita BHATTACHARYYA
When it came to iPS cells, as a developmental biologist, I thought that was science fiction. Once I wrapped my head around it, I was able to really understand the impact. IPS cells were particularly critical for my research in disease modeling, and really enabled my work to move forward.

Connie Eaves
I think the robustness of that technology — the generation of iPS cells — has revolutionized biology. First of all, it has given access to all sorts of disease cells that can be immortalized and played with. Secondly, it completely reversed historical understanding that differentiation was a one-way street. That’s upset the apple cart, scientifically, for a lot of the original concepts.

Janet Rossant
IPS cells have a big role to play in precision medicine. We are modeling diseases like cystic fibrosis, looking at the way drugs being developed for treatment and why different patients respond differently. We could potentially test ahead of time the right therapy for the right person at the right time.

Justin Brumbaugh
Jamie always told me that he estimated that it would take about 20 years to go from culturing ES cells to making iPS cells, and it's only taken about half that time. That alone, I think, shows that the science moves at a tremendous pace.
Tapping the economic potential

Gov. Tommy Thompson
In the past, Wisconsin was often an afterthought, the flyover state when it came to getting investments in the biotech industry. When I started out as governor, there was a big problem getting private equity dollars and venture capital money into the state. With Jamie Thomson and his breakthrough in embryonic stem cells, everybody had to recognize this came from Wisconsin.

Carl Gulbrandsen
In the commercial area of stem cells, from 2005 to the present, WARF has executed more than 70 commercial licenses to 47 individual entities. These entities include start-ups, some of them located here in Madison, and global pharma companies engaging in developing therapeutics.

Tom Palay
We formed two companies that eventually merged into one, Cellular Dynamics International (CDI). We had decided that the focus would be on iPS cells, and the development of both therapeutics and research tools from these cells. Jamie had both intense concentration and ability to not only understand the science, but was inherently good at the economics of the business.

James Thomson
We thought that CDI was a viable idea in that it would be selling biological tools instead of selling medical dreams.
March 9, 2009
President Barack H. Obama issued an executive order: Removing Barriers to Responsible Scientific Research Involving Human Stem Cells. This opened the door fully to federal funding for stem cell research. Alta Charo, UW–Madison professor of law and bioethics, was part of the President Obama transition team assigned to craft a new stem cell policy. Charo drafted the majority of the new executive order and attended the President’s signing ceremony.