Macrophages are specialized immune cells that can be adapted for the treatment of certain solid tumors by arming them with chimeric antigen receptors (CARs).
Tumor-associated macrophages make up about 50% of the cells in a tumor, which gives them the ability to both infiltrate and reside inside solid tumors By taking advantage of this property, macrophages equipped with CARs can specifically recognize the cancerous cells over the healthy ones, and also eliminate a subset of them in the process.
Getting to that point, however, requires lots of trial and error through genetic engineering.
New research published in the journal Stem Cell Reports investigated CRISPR-Cas9 gene editing methods to insert anti-CD2 CAR into pluripotent stem cells and produce CAR macrophages.
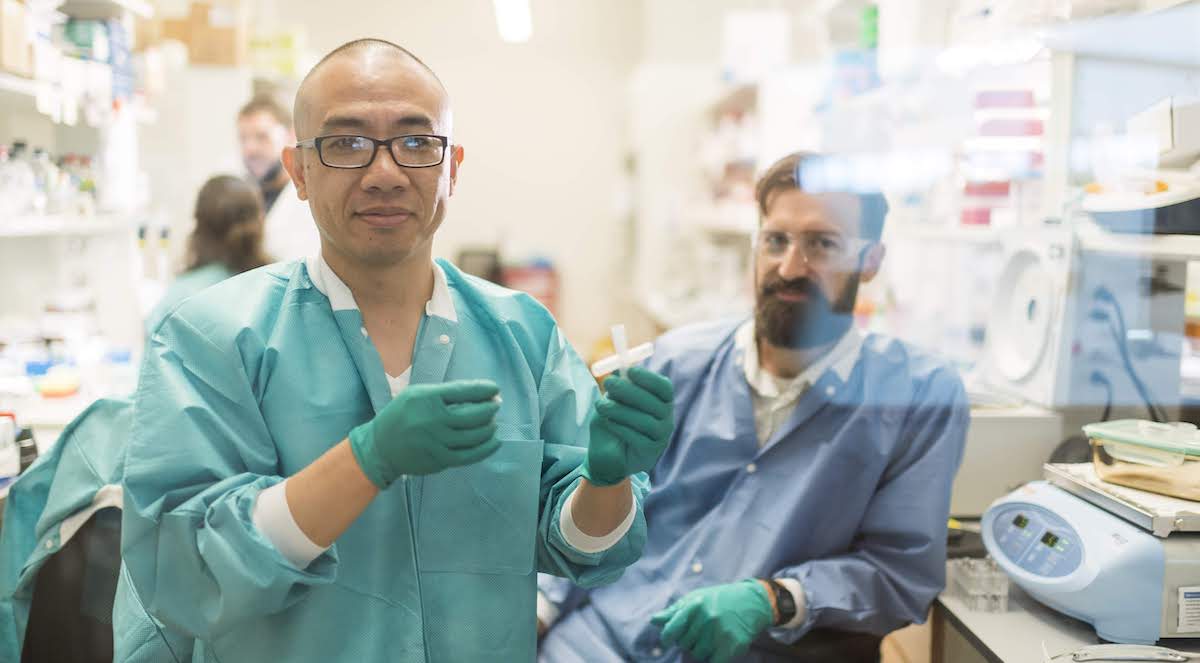
Associate scientist Jue Zhang, who has been with the Jamie Thomson Lab at Morgridge for over 11 years, took the lead in designing and carrying out experimentation, analyzing the data, and in being the primary author of the resulting publication. He expresses how these kinds of cell integrations can be very helpful in the context of cancer immunotherapy applications.
“Macrophages themselves have a limited ability to cure cancer,” says Zhang. “Once you have an anti-GD2 CAR expressed, that macrophage becomes an anti-tumor weapon.”
Cancer immunotherapy focuses on an individual’s immune system by strengthening their natural immune responses. Unlike chemotherapy or radiation, where often healthy cells are damaged in the process, immunotherapy treatment aims to enable one’s immune system to detect diseased cells right away.
Macrophages themselves have a limited ability to cure cancer. Once you have an anti-GD2 CAR expressed, that macrophage becomes an anti-tumor weapon.
Jue Zhang
To create CAR macrophages the researchers start with human pluripotent cells, which are used because of their ability to self-renew and develop, but more importantly because a human body’s supply is essentially infinite.
They are then modified with a CAR that targets GD2, a molecule that is often expressed on the surface of cancer cells.
The compelling part about GD2, says Zhang, is that “it is highly expressed in the neuroblastoma, melanoma, and other cancer cell lines,” making this a treatment that can be applied to a wider range of cancer types as a whole.
Zhang notes that it’s worth exploring ways in which to improve the so-called “killing efficiency.” Although this therapy was only concerned with the use of macrophages, the reality is that multiple cell types work together in our immune system to fight an invading pathogen. Future research might include investigating how multiple cell types, work in collaboration with each other and discerning the impacts this would have on the results.
Scientists in Regenerative Biology at Morgridge, in collaboration with researchers at UW–Madison, are motivated by the promise of the antitumor activity of modified macrophages and of cancer immunotherapy as a broader treatment option.