What is the future outlook of the COVID-19 pandemic and what does the path forward look like?
In the seventh installment of the Morgridge Institute’s Fearless Science Speaker Series on February 17, experts discussed where we are, the outlook for moving out of the crisis and into recovery, and how we can manage this new normal going forward.
Morgridge Investigator Paul Ahlquist moderated the panel discussion, which featured Tony Goldberg, professor of epidemiology at UW–Madison, Reka Sundaram-Stukel, health economist at UW–Madison, and Ryan Westergaard, chief medical officer and state epidemiologist for communicable diseases at the Wisconsin Department of Health Services.
The following is an abridged transcript of selected questions and key takeaways from the discussion. A recording of the webinar can be viewed in full above.
Paul Ahlquist: The pandemic has surprised everyone repeatedly so no one can predict the future with certainty.
What are some of the major pandemic developments that we might expect going forward?
Ryan Westergaard: We’re going to stop thinking about COVID-19 as something that can be stopped or defeated and start thinking about it in terms of in an ever present risk to health is going to continue at varying levels.
As we recover from pandemic mode, and as we build our healthcare and our medical systems to be able to respond better, we’re going to be talking about ways to keep ourselves healthy, in the face of the virus that’s going around.
I think vaccines are going to be our most potent tool. And there’s a, frankly, a communication war going on, about the benefit in the trustworthiness of vaccines. And all of us who work in public health and medicine and science need to be part of those conversations to make that the new normal because that’s how we’re going to save lives through vaccination.
With the potential for new variants, what are thoughts on those kinds of issues from the perspective of virus evolution?
Tony Goldberg: It’s important to recognize that for respiratory viruses, there’s maybe 20 or 30, that cause the common cold in people worldwide. And from what we understand, every one of those started out like we’re seeing right now with SARS-Coronavirus-2 — zoonotic transmission from an animal or, you know, a mutational event in people that rendered it nasty at the beginning and then it evolved us and we evolved it. So what we’re experiencing right now, is something that has been repeated many times over the course of recent human evolutionary history.
It’d be nice if we could tame the virus and direct its evolution so it becomes less nasty. The alternative is not great, which is that we evolved to the virus. For people to evolve, resistance to the virus means that some people will live and some people won’t. So it’d be a lot better if we tamed this virus, using the knowledge we have about viral evolution, then, if we just kind of waited around for ourselves to adapt to it.
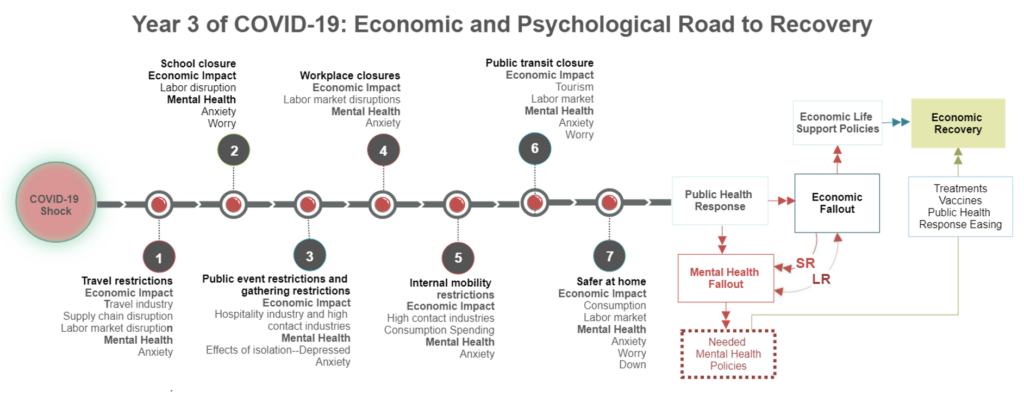
Ahlquist: The pandemic is usually discussed from a public health perspective, but Reka’s work has illuminated its economic and psychological dimensions in important ways.
What about the economic and psychological impacts?
Reka Sundaram-Stukel: I don’t think any of us, including public health officials were prepared for the magnitude of the virus. There was an unusually large disruption to our daily work life that is unanticipated. And what made it harder is that we weren’t ever sure about the duration of it. Nationally, what we are seeing is that both people who have been continuously employed, and people who have had disrupted employment are both registering unusually high levels of anxiety and depression.
And that prolonged exposure to stress like that requires additional training that we did not have before the pandemic started. In essence, we all need to incarnate today and learn how to take care of our emotional and mental well being, as if we’re starting fresh. Governments in some way cannot do very much in that capacity. So it’s the responsibility of individual workplaces, and the responsibility of individual human beings to really start investing in their well being, to really start taking ownership of it and become proactive — together, we will make sure that we will develop the muscle that we need to meet the next steps.
Ahlquist: Big challenges. Actions are needed at multiple levels.
We’ve seen tremendous impacts of the Delta and Omicron variants appearing and surging so rapidly. So everybody realizes now that viruses are not static, they evolve rapidly, as it is presumably going to continue going forward.
What should we expect and what should we do to guide the evolution of viruses?
Goldberg: So in a situation where the people are not coughing and sneezing on each other people are are wearing masks, people are practicing good social distancing and other forms of prevention, it sort of creates this pressure on the virus to, to hold back to not make you too sick, to be more benign.
We would like to change the selective pressures on the virus to drive it towards being more benign. Now, fortunately, the exact same things that help with public health are those things that will make the virus more benign. So we don’t have to do anything different than we’re doing already, we just have to recognize that there’s this added benefit.
Ahlquist: From the pandemic’s beginning, there have been challenges about what and how to communicate about masks and distancing and vaccination and other matters.
How should communication challenges be approached both by responsible communicators and by the public?
Westergaard: I think public health needs to pair our communication strategies with everything else that we do, to make sure that the public sees us as worthy of their attention and worthy of their trust. And that’s something I think is going to take years or decades to build stronger than it is now, because of the skepticism with which many people receive science these days.
People need to have the right science, the right knowledge to make good decisions.
We need to continue to communicate science effectively, but pair it with a sense of empowerment or encouragement that people have a lot of things they can do to take control and lower their own risk.
What can individuals do to address the stresses that they in their family and friends are facing?
Sundaram-Stukel: It’s important that everybody understand that this type of anxiety and depression should not be stigmatized, it should be accepted as something that is completely unusable and out of our toolbox.
You need to very firmly put on your oxygen mask before you assist any other human being in any capacity — be it financial, be it emotional, be it as a physician, be it whatever dimension of your life that is requiring you to move away from your comfort zone to an assist another person — because it’s too much for all of us.
What are we looking at in the future? What are the chances of further pandemics?
Goldberg: The chances of further pandemics are pretty much 100%. The question is when and which viruses now are. We can’t completely prevent future pandemics. What we can do is reduce their frequency and catch them sooner and be better prepared when they come.
A silver lining to the cloud of COVID-19 is that we have developed remarkable new tools, both in biomedicine and also in the social sciences and in public health to deal with it. We hopefully we won’t make the same mistakes twice.
I’m really excited about mRNA vaccines, these are potentially a game changer. They’re much easier than past vaccines to alter, to meet the challenges of novel viruses that might come into the human populations. And that’s a powerful tool if we can get people to trust them more.
Westergaard: When I think about vaccination in the triumph of mRNA vaccines, it’s not just the science and the therapeutics, but in the logistics and the distribution and the mass production, and the ethical allocation that we had to struggle with. The lives that were saved through this through mass vaccination, I think it’s changed it’s changed public health for the better.
What are you looking forward now that you find hopeful as you’re looking toward the future?
Westergaard: My hope for the future is that public health is going to expand. So that our public health workforce is much larger and more diverse, and embedded and engaged in a lot of places where we traditionally haven’t seen it. And when we’re out of a pandemic, we can still leverage a lot of those partnerships and do a lot of the things that we do across public health in a much more engaged and high impact way.
Sundaram-Stukel: We get an opportunity to reinvent ourselves a little bit, we get to be socially conscious as we make investments. My own personal hopeful trajectory is developing the field of economic psychology and looking at how mental health and economic factors are correlated with each other, and what, how to untangle the stickiness of those. After the pandemic, it’s a little bit of an opportunity to really think it through and see how these two factors are inter woven with each other and how to mitigate it.
Goldberg: One of the things that encourages me is that everybody has a better understanding of infectious disease, viruses, epidemiology, and the societal costs of disease. Everybody is now much more aware than they were before, about the fundamental links between human health, animal health and the environment. I think that in itself will prepare us better for the next one.