The National Institutes of Health (NIH) is embarking on a massive research project to shed light on early child development, including the health and developmental implications of opioid use during pregnancy. The very first task is to ensure the study — the HEALthy Brain and Child Development study (HBCD) — is on solid legal and ethical ground.
A team of Wisconsin law and bioethics scholars are supporting HBCD with a 50-state analysis of the surprisingly diverse range of laws that address substance use during pregnancy — ranging from court-ordered treatment, to loss of child custody, to possible imprisonment.
Pilar Ossorio, professor of law and bioethics at the University of Wisconsin–Madison and bioethicist-in-residence at the Morgridge Institute for Research, says the 50-state analysis is critical to protecting both research participants and researchers so this important work can move forward. Biomedical science does not have a firm grasp on all of the downstream child health impacts of substance use during pregnancy, Ossorio says, an issue made more pressing by the widespread opioid epidemic.
The Department of Health and Human Services estimated that 1.6 million U.S. citizens had an opioid use disorder in 2019. More than 48,000 deaths between June 2019 and June 2020 were attributed to opioid overdoses. In a Centers for Disease Control study, about 7 percent of women in 2019 self-reported using prescription opioid pain relievers during pregnancy, and polysubstance use during pregnancy is increasingly common.
Infants with Prenatal Substance Exposure
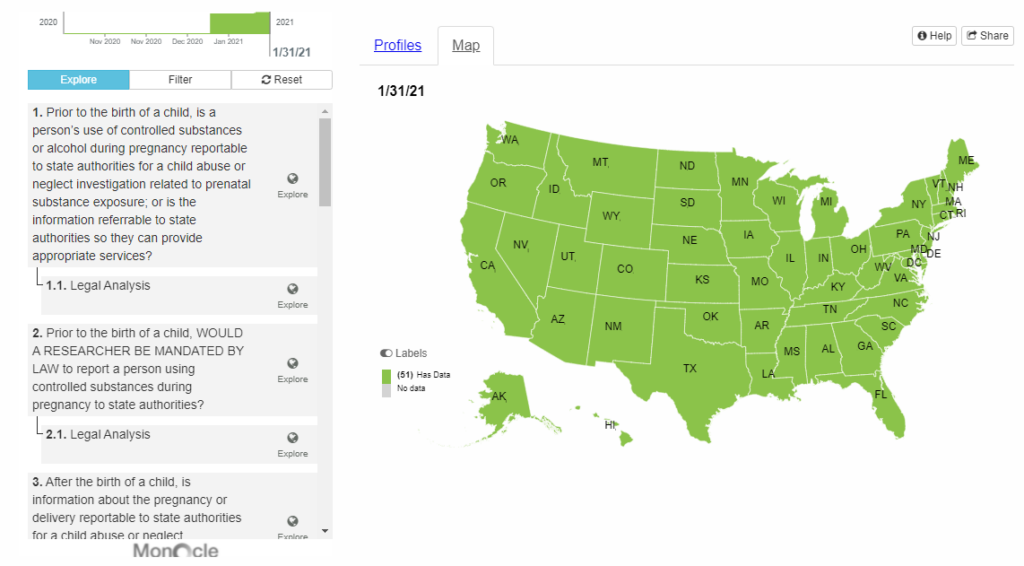
An interactive web tool highlighting key laws and policies in each state can be found here.
The HBCD study will recruit around 10,000 pregnant women, follow them through their pregnancies, and study their children through age 10. Some portion of the pregnant participants will have reported using substances (particularly opioids) at some point during their pregnancy. One goal of the HBCD will be to identify the impacts of such exposures on child development and to suggest strategies to improve health and potentially save lives.
“There is clearly a huge demand in the medical and research community for more knowledge and help in this area,” Ossorio says. “NIH has completed a very successful study looking at adolescent brain cognitive development from ages 9-10. But obviously a lot of brain, cognitive, behavioral and emotional development happens before that time.”
A longitudinal study starting with pregnant women is fraught with challenges — not the least of which are widely divergent and fast-changing state-by-state laws related to pregnancy and drug usage. “The law doesn’t look at prenatal substance exposure as a unitary kind of a thing,” Ossorio says. “Instead it has particular pieces of evidence that are used legally to define prenatal substance exposure as a kind of child abuse or neglect.”
As an example of the range of laws out there, Ossorio notes the chemical endangerment statute in Alabama. The Alabama Supreme Court has twice ruled that this statute absolutely applies to the prenatal period, including from the time of conception. “Alabama has actually prosecuted hundreds of women for prenatal chemical endangerment,” Ossorio says.

About half of the states have a statute that says that if a child has positive toxicology at or around birth, that will be defined as child abuse or neglect (maltreatment) and is reportable, Ossorio says. Using Illinois as an example, if a baby is born with positive toxicology, not only are doctors required to report this to child protective services authorities, but those authorities are required to report to a local prosecutor for potential prosecution. In almost all other forms of child maltreatment, child protective authorities are given discretion whether or not to notify prosecutors.
“And those are actually the harshest statutes,” Ossorio says. “They almost uniformly were put in place in the 1980s and 1990s and were a response to the crack epidemic, and the idea of crack babies. These came out of the view of drug use as a problem of minority populations who needed to be disciplined and controlled and penalized.”
The next spate of new laws came about in the last decade that are in direct response to the opioid epidemic. Ossorio says these are a lot less punitive. In many cases in those states, the law specifically says things like the state departments of health and human services have to be notified of the birth of a substance affected child. But this notification is not explicitly a child maltreatment report.
Another challenge in studying substance exposed newborns is that many of them will go into foster care, or into the custody of child protective services. By the time these children come out of the hospital, or shortly thereafter, they might not be in the mother’s custody anymore. Many of those children would be lost to the study, Ossorio says, so researchers will need to negotiate agreements with child protective officials to continue gathering health information on those children.
Ossorio’s project, called Promoting Resilience, is part of the 18-month first phase of the NIH project. Phase Two is expected to begin later this year. It will support the collection of a large dataset that will enable researchers to analyze brain development in opioid-exposed and non-drug-exposed infants and children across the country.
“In addition to prenatal chemical exposures, many factors can impair child development, including maternal stress during pregnancy, poverty, poor diet during the prenatal or newborn period, and adverse childhood experiences,” Ossorio says. “This larger study will help us tease apart the different causes of positive or negative developmental outcomes for children.”
