As the first responders of the innate immune system, neutrophils are specialized immune cells that circulate through the bloodstream, ready to act at any moment.
These cells are constantly being produced in bone marrow from progenitor cells that quickly mature and move out to respond to tissue damage or invading pathogens by promoting inflammation. To keep up with the demands of this important job, neutrophils require dynamic flexibility through the metabolic pathways that provide energy.
New research published in the journal Frontiers in Immunology uncovers the role of mitochondrial metabolism in neutrophils and the mechanisms that allow them to adapt under different conditions.
Mitochondria are organelles commonly referred to as the “powerhouse of the cell” due to their role in energy production.
“But neutrophils don’t use their mitochondria to maintain energy levels,” says MD/PhD candidate Jorgo Lika, first author of the study and a recent graduate from the Jing Fan Lab. “As they differentiate, they switch energy production from the mitochondria to other metabolic pathways, such as breaking down sugar through glycolysis.”

There are also fewer mitochondria present as neutrophils mature. For these reasons, Lika explains that mitochondria in neutrophils were previously thought to be unimportant and have been overlooked in the field. Additionally, neutrophils are challenging cells to grow and study in vitro, leaving much to be discovered about their metabolic functions.
“We’ve discovered that as neutrophils differentiate, the mitochondria switch roles from energy production to regulation of cell functions,” Lika says. “We wanted to see what nutrients they can use and how they use them — and more specifically, look at their usage of glucose and when they can use glucose.”
Specifically, the researchers observed dynamic shifts in the TCA cycle — a metabolic pathway in the mitochondria also known as the citric acid cycle or the Krebs cycle.
They used two neutrophil cell models, one derived from mouse progenitor cells and another from human induced pluripotent stem cells that can grow into mature neutrophils in cell culture. To study the pathway, they used a technique called isotope tracing where cells are cultured with glucose labeled with heavy carbons. They can then measure how many of these heavy carbons were picked up and incorporated into the metabolic pathways under different conditions.
As the cells differentiated from immature to mature cells, they noted a decrease in metabolites produced in the TCA cycle.
“Mitochondrial metabolism changes as the cells mature because the metabolism in those contexts is very different,” Lika says. “An immature cell is using nutrients to divide and grow versus a mature neutrophil that doesn’t divide or grow but is designed to respond to something.”
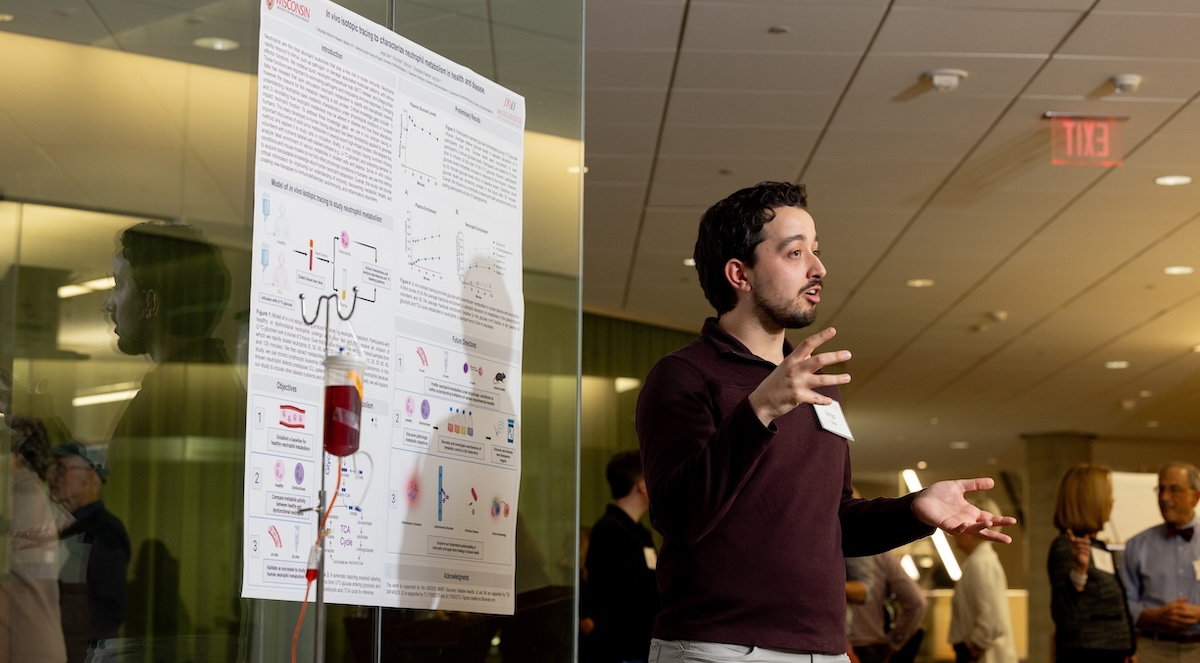
To further investigate influences on fully differentiated cells, the researchers isolated mature neutrophils from healthy human blood donors. Through the clinical portion of his MD/PhD program, Lika had the training and experience to serve as the lab’s phlebotomist and performed many of the blood draws himself.
The team found that they could reactivate the TCA cycle in mature neutrophils by introducing certain stimuli, specifically ionomycin and monosodium urate crystals, which activate calcium signaling in neutrophils.
When the neutrophils were treated with drugs that inhibited these changes in mitochondrial metabolism, it also impaired the effector functions of the cells. This suggests that the reactivation of mitochondrial metabolism is important in supporting effector functions — such as migration towards a stimulus or the release of neutrophil extracellular traps that control the spread of pathogens.
“We also collaborated with the Skala Lab to image the neutrophils and see redox metabolism changes under the different conditions,” says Lika. “It’s just a different way to look at changes in metabolism at the single cell level.”
The TCA cycle is just one of many pathways involved in immunometabolism. From different pathways in neutrophils to other immune cells like macrophages, this area of discovery is right where the Fan Lab wants to be — exploring fundamental questions to better understand the metabolic changes that impact human health.
As for Lika, his time in the Fan Lab is finished as he recently defended his thesis and completed the PhD component of his program. He is now starting his final year of medical school and will soon start preparing for residency applications.
“During my PhD and clinical rotations, I discovered my passion for dermatology and a gap in the field applying immunometabolism research to skin inflammation, especially autoimmune skin diseases,” he says. “I think I can bring in these skills and perspective — teasing out mechanisms between metabolism and cell function — all within the context of disease.”