While most COVID-19 cases are asymptomatic or mild, severe complications associated with acute respiratory distress have led to more than one million deaths worldwide in just several months.
Researchers from the Morgridge Institute for Research, the University of Wisconsin–Madison, and Albany Medical College sought to better understand the molecular factors that drive the severity of COVID-19, and offer insight into treatment options for those with advanced disease.
The collaborative study published online in Cell Systems identified more than 200 molecular features that strongly correlate with COVID-19 severity.
“To my knowledge, this the largest outcome study,” says Dr. Ariel Jaitovich, a pulmonary and critical care physician at Albany Medical Center. “I know that there are some large studies focused on the diagnostics (infected versus non-infected). We have a large group of just COVID patients, but with a very granular difference in terms of severity…that is something that I hadn’t seen.”
The team analyzed 102 blood samples from patients diagnosed with COVID-19, and 26 samples from patients with acute respiratory distress syndrome (ARDS) — but negative for COVID-19 — as controls.

“I felt like we had a unique opportunity with Ariel’s cohort that he had recruited. It was very early in the COVID epidemic here in the United States, so he was really out on the forefront of getting these types of samples from the clinic,” says Josh Coon, Morgridge metabolism investigator and professor of biomolecular chemistry at the UW–Madison School of Medicine and Public Health.
Using methods in mass spectrometry, RNA sequencing, and machine learning, the researchers explored a database of more than 17,000 different proteins, metabolites, lipids, and RNA transcripts associated with clinical outcomes.
They identified 219 molecules and genes that influence blood coagulation, vessel damage, inflammation, and other biological process reported to play a role in severe disease.
“We had to think hard about how to actually compare it to the existing data,” says Ron Stewart, Morgridge investigator and associate director of bioinformatics whose team was tasked with analyzing the transcriptome data. “What we’ve largely found is we recapitulated prior work, which is good.”

One particularly unique aspect to the study, which contributed to the robust dataset, was the team’s use of plasma samples.
“Most of the research done in proteomics, the blood samples use the serum fraction that doesn’t have the clotting factors,” says Jaitovich. “This is very important because patients with COVID-19 have accelerated clotting activity.”
A metabolite called citrate is used as a therapeutic anticoagulant to decrease the likelihood of developing clotting. Yet the study revealed that the presence of metabolic citrate decreased as patients presented with more severe illness.
“The fact that citrate is reduced in these patients will potentially indicate that the reduction facilitates the hypercoagulation phenotype that we found in these patients,” says Jaitovich.
Another molecule possibly contributing to hypercoagulation in severe COVID-19 is a protein called gelsolin, which is normally released as a response to inflammation due to cellular injury or infection. Gelsolin was also reduced in the plasma samples from people with severe disease.
In addition to biomarkers associated with hypercoagulation, the team also identified a cluster of proteins involved with blood vessel damage, with higher abundance in severe COVID-19 samples.
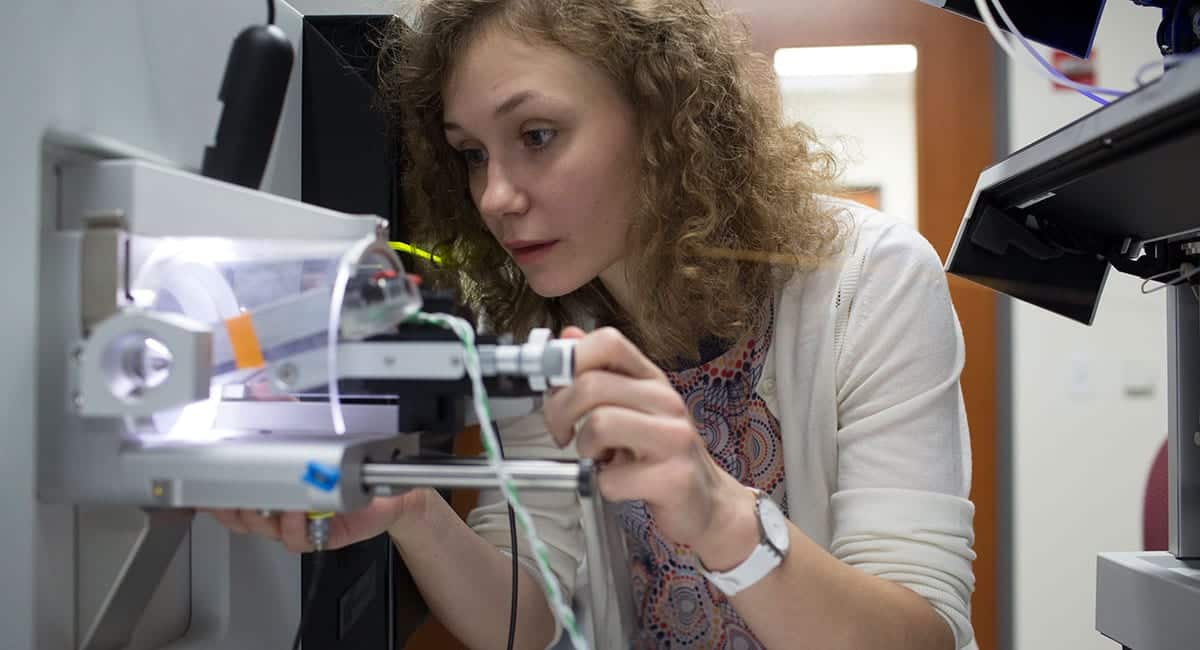
“There are all these factors upstream of the process that are actually being changed, that you need to address as much as just the process of clotting in order to manage this phenotype,” says Evgenia Shishkova, assistant staff scientist in the Coon Lab.
The analysis also revealed increased levels of proteins and upregulated genes involved in neutrophil degranulation, which has been associated inflammation, thrombosis, and the development of ARDS.
“So it seems like there’s this really strong interplay between the inflammatory response and probably these thrombotic events, which are also being seen in the COVID patients,” says Katie Overmyer, associate director of the Laboratory for Biomolecular Mass Spectrometry at UW–Madison.
Finally, the multi-omic analysis revealed a network of high-density lipoproteins—the proteins APOA1 and APOA2, and a group of lipids known as plasmalogens which act as antioxidants— were all lower in the severe COVID-19 cases.
“These aspects were not on our radar,” says Jaitovich. “The ability to merge these dimensions in one single unifying narrative allowed us to make sense of stuff that was completely obscured to us.”
And by identifying these various molecules, it opens up the potential for developing targeted therapeutics that may help alleviate disease.
“We can offer hard data for people who are specialists in all these different areas to go and maybe learn about the prospects that what they’re thinking might have an impact on COVID,” says Coon.
The researchers made the data publicly available through an interactive web tool, covid-omics.app, where the scientific community has been comparing and analyzing the data along with their own workflows.
Coon adds, “I think we’ve tried to do our best to highlight vignettes that we think are important, but the bigger impact is probably going to come from the community being able to dig into this.”