A house with no furniture
Tim Grant’s first day at the Morgridge Institute was anything but typical.
On the morning of March 16, 2020, he opened his email inbox to find several messages from fellow Morgridge scientists. Many said they weren’t coming into the office and wouldn’t be able to meet him for a welcome lunch.
After a tour of what appeared to be an empty building and a brief meeting with Brad Schwartz, the institute’s chief executive officer, they addressed the elephant in the room:
“We probably shouldn’t do the lunch, right?”
“Yeah, we won’t do the lunch.”
For Grant, his first day just happened to be the day that employees at the university — and residents statewide in Wisconsin — were told to work from home. It was the first day when many accepted the COVID-19 pandemic was here.
“That was the worst day possible to start,” Grant laughs, reflecting on the uncertainty of that day.
Grant, a native of London, England, had just moved 800 miles from the Janelia Research Campus at the Howard Hughes Medical Institute in Washington, D.C. He was ready to start his lab as an investigator in the John W. and Jeanne M. Rowe Center for Research on Virology at Morgridge.
Soon, he imagined, he would start hiring trainees who specialize in computational approaches for solving molecular structures, such as cryo-electron microscopy (cryo-EM) — a highly-complex, critical tool that researchers use to see the atomic structure of viruses, some of the smallest living things on earth.
Scientists like Grant are trained to embrace the unknown. They follow science, fearlessly, to ask questions and make progress in understanding what we don’t know, and why.
Grant faced the uncertainty of a new job. His family, including two young children, was adjusting to their new city, and a new house with empty rooms. They had planned to shop for furniture in Madison, but of course, that didn’t exactly pan out during the shutdown.

“When you start a new position you have amazing drive and energy to get stuff done, you know, it’s all new and exciting — and I had all that,” Grant says. “I had all that, but nothing to do with it.”
Despite the limitations that the COVID-19 pandemic placed on the workplace, Grant was able to make early progress. He was able to return to work and slowly begin hiring members of his research team.
The COVID-19 pandemic isn’t the first time that humanity has faced a major public health challenge, and it certainly won’t be the last.
But these challenges haven’t stopped scientific progress.
COVID-19 Pandemic Timeline
December 31, 2019
First reports of mystery pneumonia-like disease in Wuhan, China
US Deaths: 0 | Worldwide Deaths: 0
January 11, 2020
First draft of the novel coronavirus genome sequence is made publicly available
US Deaths: 0 | Worldwide Deaths: 1
February 11, 2020
COVID-19 becomes the official name for the novel coronavirus disease
US Deaths: 0 | Worldwide Deaths: 1,129
March 11, 2020
WHO declares COVID-19 an international pandemic
US Deaths: 38 | Worldwide Deaths: 4,637
March 13, 2020
US declares a national emergency (instates travel bans and stay at home orders)
US Deaths: 47 | Worldwide Deaths: 5,447
March 27, 2020
CARES Act is signed into law (the largest economic recovery package in history)
US Deaths: 2,176 | Worldwide Deaths: 28,951
April 30, 2020
Operation Warp Speed launches to expedite production of a vaccine
US Deaths: 65,783 | Worldwide Deaths: 240,617
July 23, 2020
Pfizer and BioNtech announce vaccine distribution plan
US Deaths: 150,472 | Worldwide Deaths: 706,300
August 15, 2020
Saliva testing approved by FDA
US Deaths: 176,979 | Worldwide Deaths: 851,820
December 11, 2020
Pfizer-BioNTech vaccine receives Emergency Use Authorization
US Deaths: 311,095 | Worldwide Deaths: 1,700,983
December 18, 2020
Moderna vaccine receives Emergency Use Authorization
US Deaths: 330,608 | Worldwide Deaths: 1,784,257
February 22, 2021
Over 500,000 deaths in the US
US Deaths: 520,104 | Worldwide Deaths: 2,604,359
February 27, 2021
Johnson & Johnson vaccine receives Emergency Use Authorization
US Deaths: 531,192 | Worldwide Deaths: 2,655,040
March 19, 2021
100 million vaccinations administered in the US
US Deaths: 559,395 | Worldwide Deaths: 2,833,104
April 8, 2021
Alpha (B.1.1.7) variant becomes the dominant strain in the US
US Deaths: 576,732 | Worldwide Deaths: 3,035,622
April 19, 2021
All US adults are eligible for COVID-19 vaccines
US Deaths: 584,430 | Worldwide Deaths: 3,166,423
April 29, 2021
US reports significant drop in cases
US Deaths: 592,155 | Worldwide Deaths: 3,307,398
May 26, 2021
CDC reports that breakthrough infections are rare
US Deaths: 608,347 | Worldwide Deaths: 3,661,954
June 23, 2021
Delta variant concerns rise
US Deaths: 619,994 | Worldwide Deaths: 3,924,236
July 7, 2021
Delta variant becomes the dominant strain in the US
US Deaths: 622,594 | Worldwide Deaths: 4,032,884
August 23, 2021
Pfizer-BioNTech vaccine receives full FDA approval
US Deaths: 650,645 | Worldwide Deaths: 4,457,570
The great pivot: the desire to make a difference
By spring 2020, the Discovery Building contained only a small fraction of its total staff, those who needed direct access to wet labs to continue research.
Everyone else was suddenly at home — surrounded by monitors and logging into video calls, usually just out of earshot of spouses, roommates, children or pets.
How would collaborative work continue when public health mandates required social distancing?
And even more essential for Morgridge: How can a biomedical research institute devoted to the long view of science — big questions that may take decades to solve — make contributions to fighting the disease that suddenly upended the world?
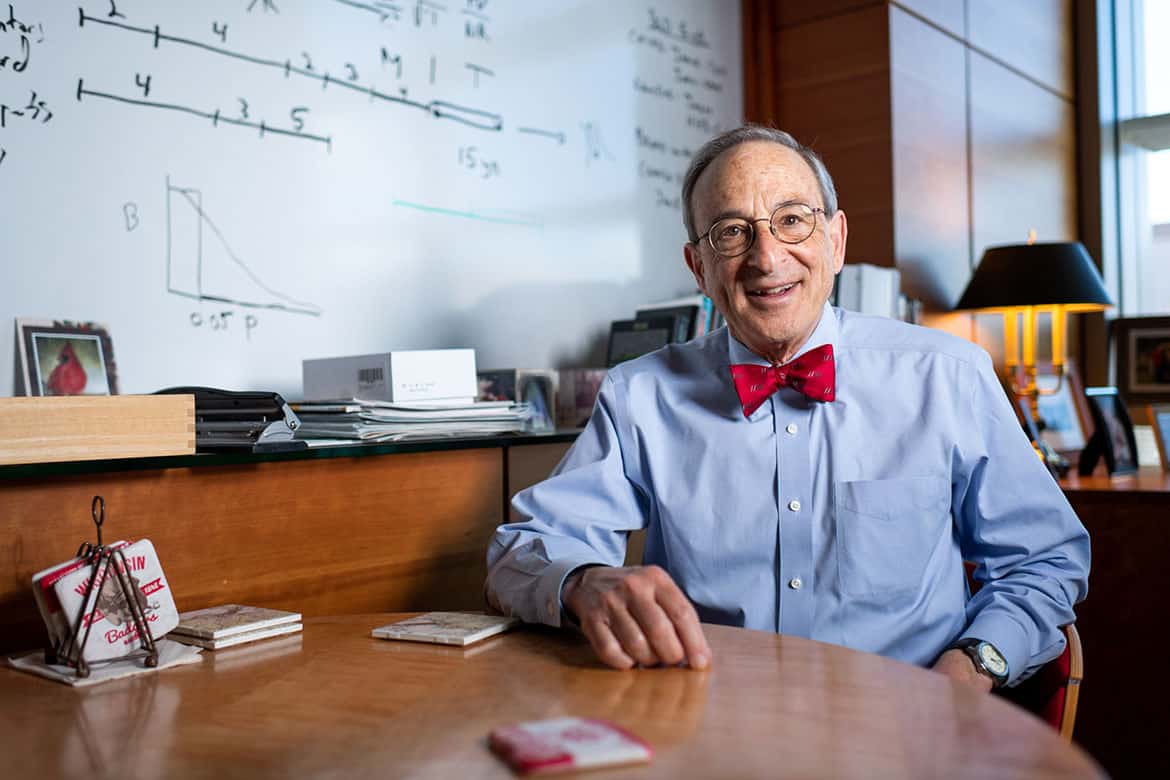
Josh Coon, a Mogridge investigator in metabolism and professor of biomolecular chemistry at the UW–Madison School of Medicine and Public Health, wrestled with this question early in the pandemic.
He couldn’t shake the idea that his team could do something, anything to help. He wanted to find a way to bring some of his team safely back to the lab.
“We’re not virologists. This is not our thing. But we’re all thinking, ‘How do you pivot to contribute?’” Coon remembers.

What Coon did have was a state-of-the-art mass spectrometry lab equipped by major technology investments from the National Institutes of Health (NIH). This innovative technology helps scientists understand disease, metabolism, and the intricate complexity of our body’s proteins, lipids, and molecules.
“I just thought to myself, look, we’ve got $8 million worth of stuff and it’s just sitting there and it’s not doing anything. And wouldn’t it be great if we could find a way to try and use it for something that might be helpful for the pandemic,” he says. “It doesn’t mean that it’s going to deliver something that’s a cure, but it can be of use and help shed light on it and help basic science.”
Early in 2020, Coon was approached by a former collaborator, Dr. Ariel Jaitovich, a pulmonary and critical care physician at Albany Medical Center in New York — one of the major hotspots during the first wave of the COVID-19 pandemic.
The Coon Lab’s expertise in developing and using mass spectrometry analytical methods, paired with the bioinformatics expertise from Morgridge Investigator Ron Stewart, helped Jaitovich answer the question: Why do some COVID-19 patients get really sick and die, while others only have mild symptoms?
The team produced an interactive, public web tool to help researchers navigate the unknowns of the disease. The Coon Lab estimates that about 1700 users have accessed the resource, demonstrating the desire for data accessibility and transparency to advance COVID-19 research.
Finding order in the chaos
Tony Gitter, a Morgridge investigator specializing in research computing and machine learning applications for virology, leveraged his expertise with the Manubot software tool he codeveloped to chronicle the pandemic in real-time. The scientific literature surrounding COVID-19 was exploding and researchers needed a tool to quickly catalog and review the vast amounts of COVID-19 data.
“Scientists were very, very eager to contribute and help, and we were all desperate to learn anything that might help with treatment — but there wasn’t amazing coordination there,” says Gitter. “There’s this parallel to Wikipedia, just continually updating entries that massive teams can collaborate on.”
Fifty scientists and researchers made contributions to the Manubot collaboration. The developmental journey of the entire project will be published as a seven-part special issue of mSystems, to showcase the power of collaboration and how new approaches to science must evolve.
As the mountain of scientific research quickly piled up during the pandemic, Morgridge bioethicist in residence Pilar Ossorio argued that urgency shouldn’t trump sound science.
Ossorio, also a professor of law at UW–Madison, has been a guiding voice around ethical discussions surrounding everything from drug repurposing, clinical trials and vaccine distribution.
Science and policy go hand-in-hand during a public health crisis. As scientists, researchers and policy makers navigate the unknown and work toward solutions, Ossorio poses the question: “What is reasonable in this situation?”
Basic research is fundamental to advancing human health. Morgridge scientists have been working to understand the depths of biology to help fight deadly diseases like cancer, HIV/AIDS, and many other disorders.
And that work has contributed meaningfully to the global fight against COVID-19.
For Paul Ahlquist, that work has been persistent, measured, and tirelessly centered on one important question — how do viruses replicate and interact with their hosts?
Ahlquist, the director of the John W. and Jeanne M. Rowe Center for Research on Virology and professor of oncology and molecular virology at UW–Madison, has spent much of the last decade revealing the molecular structures of important viral “protein machines” inside of virus-infected cells.
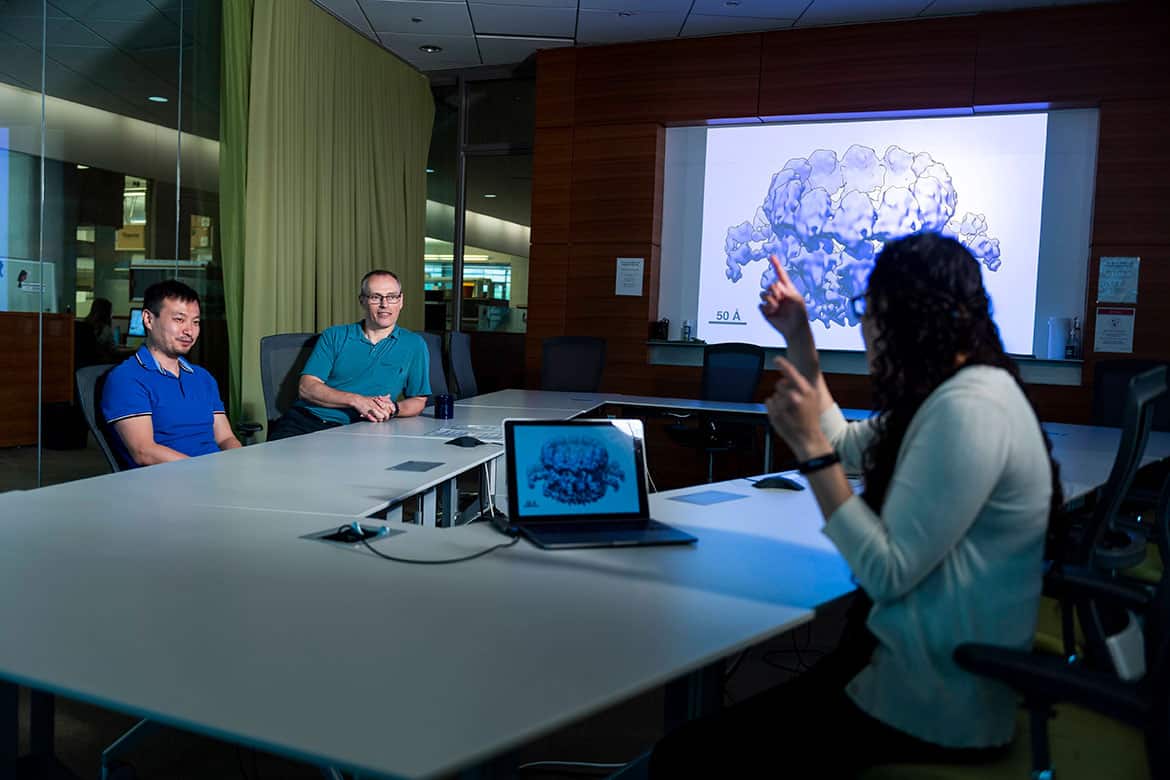
His team, in collaboration with Tim Grant, has used revolutionary cryo-EM approaches to first reveal and now produce increasingly detailed structural images of a crown-like viral RNA replication complex responsible for genome replication in the class of viruses that includes SARS-CoV-2.
The near atomic-level detail reveals valuable insights into how the replication complex assembles and functions — a foundational discovery needed to develop antiviral approaches.
“There are hundreds of structures, different parts of the coronavirus, that have been solved by cryo-EM in the last year,” says Grant. “As a field, cryo-EM has really provided a lot of coronavirus knowledge.”
The Ahlquist Lab has been in their element during the pandemic, but that wasn’t true for many scientists working in other fields of biology.
Here you have all of these people who are basic researchers who made a change in what they were doing, because they knew society needed it. To me, this was a huge win. It demonstrated their commitment: “here’s a chance for me to do something good, and I’m going to do it.”

Brad Schwartz
Chief Executive Officer
Phil Newmark’s regenerative biology lab found a way to repurpose their work for the benefit of pandemic research. The Newmark Lab was on track to begin a project using nanobodies to study parasitic flatworms, until COVID-19 stopped them before they could start.
So Newmark and John Brubacher, assistant scientist, altered their project using nanobodies to bind to the SARS-CoV-2 spike protein as a target for therapies that could stop infection.
Other Morgridge scientists quickly recognized how their research questions could be recalibrated to help with the pandemic crisis. The research computing world was especially ripe.
Postdoctoral researcher Kalpana Raja, a co-developer of a powerful literature-based search tool called TripleMiner, explored a way to speed up the race to identify existing drugs that could help treat COVID-19 patients. She trained TripleMiner on pre-existing conditions that make the disease more deadly – such as obesity, diabetes and hypertension — to find “hits” for drugs that work across multiple diseases, and could be good candidates for treating COVID-19.
The Morgridge and UW–Madison Center for High-Throughput Computing (CHTC), which serves the data science needs of hundreds of UW–Madison scientists annually, put out a special call in spring 2020 for projects related to COVID-19, resulting in five major collaborations. One of the biggest projects used HTC to help Wisconsin public health officials track down viral variants sickening people across the state — shaving critical time off the process.
“Here you have all of these people who are basic researchers who made a change in what they were doing, because they knew society needed it,” says Schwartz. “To me, this was a huge win. It demonstrated their commitment: ‘here’s a chance for me to do something good, and I’m going to do it.’”
How we changed as scientists
“We tend to pigeonhole science. We say, ‘This is basic research, this is translational research, this is applied research,’” says Schwartz. “We make a point of saying that we focus on basic research, but I don’t want the message to stop there.”
Because collaboration — at all stages of science — is essential, he adds.
The COVID-19 pandemic only served as an even greater motivator to make science more open, transparent, and accessible.
Gitter recalls his collaboration with Manubot, the tool to help catalog scientific publications in real-time during the pandemic.
“We’re in a crisis, let’s use the tools and knowledge we have to actually make progress,” he says. “That’s the primary, and maybe the only goal. Openness really helped accelerate things.”
The explosion of scientific literature related to COVID-19 and SARS-CoV-2 — more than 50,000 papers in PubMed in the course of a year — clearly demonstrated that scientists worldwide were eager and ready to collaborate and share knowledge.
Many took to immediately publishing early manuscripts on preprint servers. These online databases house research and scholarly papers that have not yet gone through the scientific peer-review process (the ‘gold standard’ for academic publishing).
And that shift wasn’t necessarily a bad thing at all, adds Gitter.
“A lot of people like me think that preprint servers are healthy for science,” he says. “This is a way we should be sharing our work and getting feedback early.”
Stewart, who leads a team of data scientists and contributed to the Albany Medical collaboration, said the shift to preprints and data sharing was immediate and quick in his field.
“When I first started in science, people kept everything quiet because they didn’t want to be scooped,” he says. “Now, the attitude is, ‘Let’s put it out on bioRxiv so we can stake our claim to it!’”
In a pandemic dominated by misinformation, it’s possible that preprints or early manuscripts could have contributed inadvertently to the explosion of inaccurate, misleading or false data or claims.
But among research and scholarly communities, that just didn’t pan out in the pandemic, says Gitter. In fact, the explosion of preprints related to the pandemic showed the system works.
“Scientists pushed back really hard with some of the claims about the evolution of the virus, and origins of the virus that were not scientifically grounded,” Gitter says, recalling the early months of the pandemic in 2020. “Misinformation was out there, but it didn’t linger and propagate too long.”
But for Stewart, preprints are just one piece in science. The most integral part is the collaboration, like lending his team’s expertise in RNA sequencing at a moment when clinicians in New York state needed it most.
“I need collaborators, because I’m just a computational person,” Stewart says with a laugh, gesturing to one of his many monitors around his desk. “I need people who will help me test predictions and work with me to refine the biological validity of the algorithms we’re developing.”
For Schwartz, the message is (and was) clear, even before the pandemic: great ideas come from collaboration and working together. The pandemic underscored just how much the scientific community needs it.
How we changed personally
“We’re in this together,” wrote Schwartz in March 2020, just a few days into the shutdown. And he meant it.
The initial two-week lockdown turned into months. And for many teams at the institute, the short-term transition started to look like a challenging long-term reality.
Melissa Skala, an engineer specializing in biomedical imaging, says she’s followed a very specific mantra, and it was one she repeatedly told her team: prioritize your health and well-being — anything else is a bonus.
Skala mentors a team of 17 people in her role as a Morgridge Investigator and professor of biomedical engineering at UW–Madison.
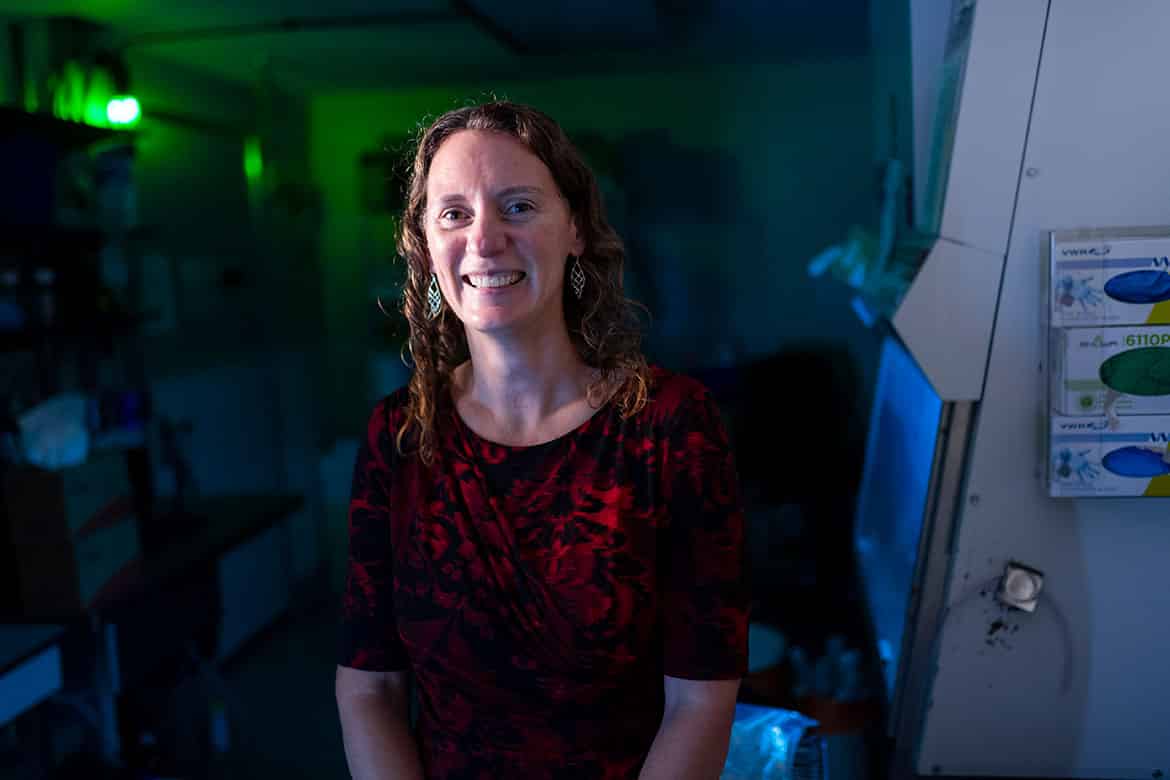
“A lot of my team was really stressed about the uncertainty,” she recalls. “I always reminded them what they already accomplished, and what they could do with what they’d accomplished. We took it day by day and we tried to be positive.”
One upside to being at home, she adds, is that many of her trainees were able to finish long standing projects that had been on the backburner. While the lab was closed, her team had time to review and process research data and write publications. In total, her lab contributed to 23 publications since the pandemic.
“I think the pandemic forced me to be a very go-with-the-flow person,” says Dan Gil, an alumnus of the Skala Lab, reflecting on how it impacted his last months in the lab.
That mentality probably helped when Gil, who finished his Ph.D. during the height of the pandemic, presented his thesis defense via Zoom to an audience of about 50 people.
“In a way, it was actually kind of a blessing in disguise,” he says. “I have family and friends scattered across the U.S., and in the old days, pre-pandemic they would’ve had to come to Madison if they wanted to see me defend. But they were all able to be there. So it was a really great way to find some connection.”
Gil also found flexibility in landing his next appointment — a postdoctoral research position at the University of Texas at Austin — since he could do Zoom interviews instead of taking time off to fly to different locations.
He says that Skala taught him how to be productive during a time of uncertainty and to embrace work-life balance.
“Those are two things I know are going to be important for me and my future career,” Gil says. “Melissa has always promoted work-life balance, she really exemplifies that. So modeling that in my own life has really improved my mental health.”
The pandemic has been a nice way to refocus, and I think that can be good — not only for work, but for life. I’m living at a totally different pace now than I was before the pandemic, and maybe it was a good thing to take a step back.

Melissa Skala
Investigator, RRF Daniel M. Albert Chair in Biomedical Engineering
In the larger world of academic research and teaching, there may be signs of change — a recalibration of what milestones matter in a scientist’s career.
Gitter saw that first-hand. He submitted his application for tenure at UW–Madison during the pandemic.
During that process — which was approved in April 2021 — he had a few surprises along the way.
“The focus wasn’t on the number of publications, or publication in a certain journal. It was more about: What is the narrative of your science and how has it had an impact?” he says.
And in that moment Gitter says he felt validated for working on projects like Manubot during the pandemic. It reinforced that the greater good in science is just as valuable — if not more — than the traditional “publish or perish” mindset in research.
Skala, whose team has been returning to in-person work, can’t help but remember how important it was to take a break and step back. There’s a silver lining there.
“The pandemic has been a nice way to refocus, and I think that can be good — not only for work, but for life,” Skala says. “I’m living at a totally different pace now than I was before the pandemic, and maybe it was a good thing to take a step back.”
A better model for public understanding
Unlike previous pandemics, COVID-19 is likely the first where the spread of information (and misinformation) might be just as viral as the disease.
Science has played a huge role in helping to curb the pandemic. But the way we talk about science is just as important. And that’s been challenging — really challenging. The virus is mutating. People’s actions are changing. Policies and public health recommendations are inconsistent. Suddenly, the entire pandemic ecosystem has evolved (and will again, and again).
For people outside of the science world, it can look like science doesn’t work.
“People find that very frustrating,” says Skala. “The pandemic is a perfect example of that. At first, we didn’t know what we were dealing with. So we had to react and adjust, react and adjust. And that’s exactly how the scientific method works. It doesn’t just give you the ‘right’ answer.”
Skala says all scientists have to get better at explaining the process of science: it’s trial and error. But it works.
In one year, we witnessed science at work through the successful development of COVID-19 vaccines at an unprecedented speed. But that speed was only possible because of decades of basic science research.
“Five years ago, the vaccines probably wouldn’t have been developed so quickly,” says Ahlquist, much of whose lab works on positive-strand RNA viruses, a large class of deadly viruses that includes SARS-CoV-2.
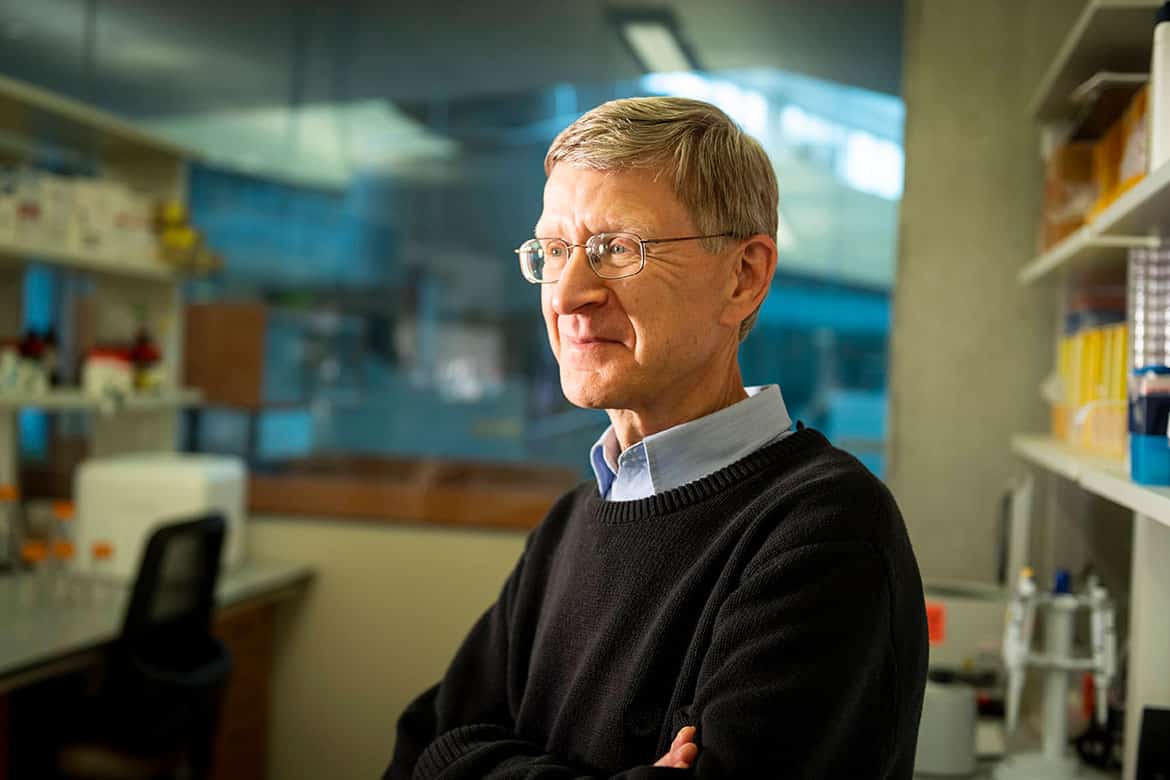
Both Pfizer-BioNTech and Moderna developed messenger RNA (mRNA) vaccines — the first application of mRNA technology in this context. The technology has been a tremendous tool in the arsenal against COVID-19, adds Ahlquist, noting that they give rapid-response possibilities that have not yet been available in the fight against other infectious diseases.
“Nobody could have predicted back when they first discovered mRNA that this would happen,” says Schwartz. “This has been a world saver — not a life saver, a world saver.”
The COVID-19 vaccines are truly a story of hope and awe.
Scientists across the world took incremental steps over decades to better understand mRNA and set the stage for an unprecedented moment in scientific history — the development of effective vaccines approved for emergency use authorization within a year.
But clearly, that story has been difficult to communicate, since only about half of the US population is fully vaccinated.
Not only that, but the scientific process is built on uncertainty. You start with a question, and the answer may not be obvious — or what you intended to find. And that’s the point. But it’s a challenging message to communicate to the outside world.
Since the pandemic began, we’ve learned so much about how the virus is transmitted, who it affects, what the long term implications of disease might be, and we’ve had to adjust our response based on new knowledge. That’s the scientific process — and there is still much more to learn.
“I’m trying to focus on the uncertainties in science, and how that’s a natural and healthy part of the process,” says Skala. “Science is continually changing, and it’s complex. Our job is to not take things for granted.”
For Schwartz, who is also a practicing medical doctor at UW Hospital, he sees two roles for scientists: on one hand, scientists are scholars working together to advance human health, but they are also citizens who can help communities better understand the scientific process (and why it matters).
“I’m a scientist because I love puzzles,” he says. “Individual scientists can take every interaction that they have with non-scientists as an opportunity to show them you’re a regular person. And that just like them, you do things that you hope are helpful to other people.”
Endgame: the space race against viruses
Before COVID-19, most known coronaviruses typically caused mild respiratory illness, like the common cold. But the SARS and MERS outbreaks in 2002 and 2012, respectively, showed that coronaviruses could have more severe implications.
Many scientists imagined an influenza pandemic, especially given the ever-evolving nature of influenza viruses which requires annual reformulation of vaccines to prevent large-scale epidemics. And the public had recent memories of dangerous outbreaks of Ebola and Zika viruses, in addition to decades of an insurmountable effort to globally slow the spread of HIV/AIDS.
But the startling — and scary — reality is that global pandemics will continue.
“COVID-19 is not a one-off,” says Ahlquist, who has spent several decades studying viruses, including the coronavirus family. “The frequency of these events has increased for reasons we understand.”
The human population continues to grow at unprecedented rates. We’re exploiting natural resources and encroaching on natural environments with animals who harbor viruses. When these pathogens come in contact with humans, they can sometimes jump quickly into human hosts, mutate, and spread with devastating impacts.
“We are often asked, ‘Why don’t you just work on the important viruses?’ But the lesson of the last 100 years is: everything is important,” says Ahlquist. “Nearly every time the world has been hit with a new viral plague, it’s been from a class of viruses that had not previously been linked to serious human disease.”
We are often asked, ‘Why don’t you just work on the important viruses?’ But the lesson of the last 100 years is: everything is important. Nearly every time the world has been hit with a new viral plague, it’s been from a class of viruses that had not previously been linked to serious human disease.

Paul Ahlquist
Director, John W. and Jeanne M. Rowe Center for Research in Virology
Vaccines and antiviral treatments are important tools to combat viral threats. But these tools are only targeting a small fraction of how a virus operates, and more importantly, how it replicates and spreads.
Take COVID-19: the current vaccines and treatments are largely targeted against one protein of the virus — the external spike protein.
“That protein is encoded by only about 12 percent the virus’s genome. By comparison, we’re giving much less attention to the other, nearly 90 percent of viral genes that could also be valuable control targets,” Ahlquist says. “There might be better targets that are less likely to evolve variants. And targeting multiple viral factors at once is an important way to get stronger, more stable protection.”
To stop the next viral pandemic, scientists need to gain deeper knowledge of how viruses like coronavirus can replicate, infect hosts and cause disease.
“We need a ‘space race’ against viruses,” Ahlquist says. “We simply need to understand them better.”
Fundamental research in virology, up until this moment, has revealed the tremendous diversity among viruses. But this research has also unveiled functional similarities among viruses, such as how they operate and might be controlled.
“With more understanding, we can say, ‘Aha! They all have factor X and they all use process Y. Now that we know what X and Y are, we can do something about them,” Ahlquist says. “Some of these commonalities could be used as targets for more broad-spectrum control.”
The COVID-19 pandemic has only highlighted — critically — that we need to double down on basic research to better understand, prevent, and stop the next deadly outbreak from an unknown foe.
Economic impacts of COVID-19
- $16 trillion
- Estimated cost of COVID pandemic on U.S. economy
- $5.89 billion
- Annual budget for the NIH National Institute of Allergy and Infectious Disease (2020)
- $10,966
- Annual health care costs per person in U.S. (2019)
- $2 trillion
- Cost to U.S. of Iraq and Afghanistan wars over past 20 years
- $778 billion
- Annual budget for U.S. military (2020)
- $300
- Estimated annual U.S. expenditures per person on public health and prevention
To date, the virus has claimed more than 4.7 million lives. Here in the United States, we are home to 4 percent of the world’s population but responsible for 14 percent of all COVID-19 deaths.
And many billions more across the world have been devastated by the economic toll of the pandemic. Now, more than ever, is the time to invest in fundamental research.
“COVID shows us the level of the threats that viruses pose, and recent history shows us that we need to act to protect against the next pandemics,” Ahlquist says. “This is not a gamble. Economic analyses show that basic research provides an unmatched, enormous return on investment and is perhaps is the single best thing that society can put money toward.”
Such investment in basic research could help understand the extent, diversity and function of viruses out there. It could advance rational approaches to control them — and improve upon existing approaches, like mRNA technologies. It could bolster distribution efforts, both nationally and globally.
“We have a crucial need. We have clear pathways to address that need,” says Ahlquist. “The final step is: let’s get going.”

